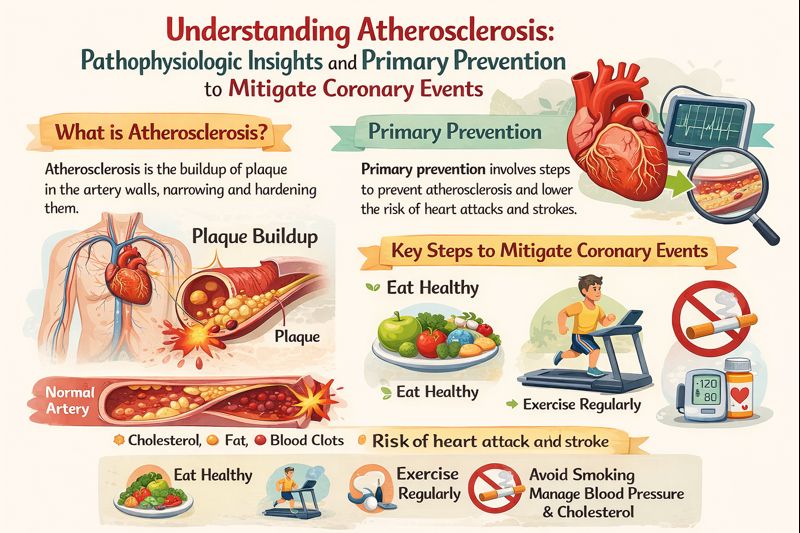
Understanding Atherosclerosis: Pathophysiologic Insights and Primary Prevention to Mitigate Coronary Events
DOI:
https://doi.org/10.65280/panhsj.v1i1.16Keywords:
Atherosclerosis, LDL, Inflammation, Acute Coronary Syndrome, Acute Myocardial InfarctionAbstract
Atherosclerosis represents the fundamental pathological process underlying ischemic heart disease, particularly acute coronary syndrome, and remains a major cause of cardiovascular morbidity and mortality worldwide. Its development is driven by a complex interplay of endothelial dysfunction, lipid deposition, inflammatory activation, and fibrous plaque formation, culminating in plaque rupture and subsequent coronary flow obstruction. In this paper, we comprehensively explore the pathophysiological mechanisms of atherosclerosis and discuss potential preventive strategies aimed at attenuating its progression and reducing the burden of ischemic heart disease.
References
[1]. Herrington W, Lacey B, Sherliker P, Armitage J, Lewington S. Epidemiology of Atherosclerosis and the Potential to Reduce the Global Burden of Atherothrombotic Disease. Circ Res. 2016;118(4):535–46. https://doi.org/10.1161/CIRCRESAHA.115.307611 DOI: https://doi.org/10.1161/CIRCRESAHA.115.307611
[2]. Qanitha A, Qalby N, Amir M, Uiterwaal CSPM, Henriques JPS, de Mol BAJM, Mappangara I. Clinical Cardiology in South East Asia: Indonesian Lessons from the Present towards Improvement. Global Heart. 2022; X(X): X. DOI: https://doi.org/10.5334/gh.1133 DOI: https://doi.org/10.5334/gh.1133
[3]. Jebari-Benslaiman S, Galicia-García U, Larrea-Sebal A, Olaetxea JR, Alloza I, Vandenbroeck K, et al. Pathophysiology of Atherosclerosis. Int J Mol Sci. 2022;23(6):1–38. https://doi.org/10.3390/ijms23063346 DOI: https://doi.org/10.3390/ijms23063346
[4]. Björkegren JLM, Lusis AJ. Atherosclerosis: Recent developments. Cell. 2022;185(10):1630–45. https://doi.org/10.1016/j.cell.2022.04.004 DOI: https://doi.org/10.1016/j.cell.2022.04.004
[5]. Casino PR, Kilcoyne CM, Quyyumi AA, Hoeg JM, Panza JA. The role of nitric oxide in endothelium-dependent vasodilation of hypercholesterolemic patients. Circulation. 1993;88(6):2541–7. https://doi.org/10.1161/01.CIR.88.6.2541 DOI: https://doi.org/10.1161/01.CIR.88.6.2541
[6]. Panza JA, Casino PR, Kilcoyne CM, Quyyumi AA. Role of endothelium-derived nitric oxide in the abnormal endothelium- dependent vascular relaxation of patients with essential hypertension. Circulation. 1993;87(5):1468–74. https://doi.org/10.1161/01.CIR.87.5.1468 DOI: https://doi.org/10.1161/01.CIR.87.5.1468
[7]. Alexander RW. Hypertension and the Pathogenesis of Atherosclerosis Oxidative Stress and the Mediation of Arterial Inflammatory Response: A New Perspective. Am Heart J. 1995;25(2):155–61. DOI: https://doi.org/10.1161/01.HYP.25.2.155
[8]. Peng R, Luo M, Tian R, Lu N. Dietary nitrate attenuated endothelial dysfunction and atherosclerosis in apolipoprotein E knockout mice fed a high-fat diet: A critical role for NADPH oxidase. Arch Biochem Biophys [Internet]. 2020;689:108453. Available from: https://doi.org/10.1016/j.abb.2020.108453 doi: 10.1016/j.abb.2020.108453 DOI: https://doi.org/10.1016/j.abb.2020.108453
[9]. Blekkenhorst LC, Bondonno CP, Lewis JR, Devine A, Woodman RJ, Croft KD, et al. Association of dietary nitrate with atherosclerotic vascular disease mortality: A prospective cohort study of older adult women. Am J Clin Nutr. 2017;106(1):207–16. https://doi.org/10.3945/ajcn.116.146761 DOI: https://doi.org/10.3945/ajcn.116.146761
[10]. Khambata RS, Ghosh SM, Rathod KS, Thevathasan T, Filomena F, Xiao Q, et al. Antiinflammatory actions of inorganic nitrate stabilize the atherosclerotic plaque. Proc Natl Acad Sci U S A. 2017;114(4):E550–9. https://doi.org/10.1073/pnas.1613063114 DOI: https://doi.org/10.1073/pnas.1613063114
[11]. Tian J, Gu X, Sun Y, Ban X, Xiao Y, Hu S, et al. Effect of statin therapy on the progression of coronary atherosclerosis. BMC Cardiovasc Disord. 2012;12. https://doi.org/10.1186/1471-2261-12-70 DOI: https://doi.org/10.1186/1471-2261-12-70
[12]. Almeida SO, Budoff M. Effect of statins on atherosclerotic plaque. Trends Cardiovasc Med [Internet]. 2019;29(8):451–5. Available from: https://doi.org/10.1016/j.tcm.2019.01.001 doi: 10.1016/j.tcm.2019.01.001 DOI: https://doi.org/10.1016/j.tcm.2019.01.001
[13]. Vaughan CJ, Gotto AM, Basson CT. The evolving role of statins in the management of atherosclerosis. J Am Coll Cardiol. 2000;35(1):1–10. https://doi.org/10.1016/S0735-1097(99)00525-2 DOI: https://doi.org/10.1016/S0735-1097(99)00525-2
[14]. Aviram M, Dankner G, Cogan U, Hochgraf E, Brook G. Lovastatin Inhibits Low-Density Lipoprotein Oxidation and Alters Its Fluidity and Uptake by Macrophages: In Vitro and In Vivo Studies. Metab Clin Exp. 1992;41(3):229–35. https://doi.org/10.1097/00006534-198103000-00132 DOI: https://doi.org/10.1016/0026-0495(92)90263-A
[15]. Chen L, Haught WH, Yang B, Saldeen TGP, Parathasarathy S, Mehta JL. Preservation of endogenous antioxidant activity and inhibition of lipid peroxidation as common mechanisms of antiatherosclerotic effects of vitamin E, lovastatin and amlodipine. J Am Coll Cardiol [Internet]. 1997;30(2):569–75. Available from: http://dx.doi.org/10.1016/S0735-1097(97)00158-7 doi: 10.1016/S0735-1097(97)00158-7 DOI: https://doi.org/10.1016/S0735-1097(97)00158-7
[16]. Weber C, Erl W, Weber KSC, Weber PC. HMG-CoA reductase inhibitors decrease CD11b expression and CD11b- dependent adhesion of monocytes to endothelium and reduce increased adhesiveness of monocytes isolated from patients with hypercholesterolemia. J Am Coll Cardiol [Internet]. 1997;30(5):1212–7. Available from: http://dx.doi.org/10.1016/S0735-1097(97)00324-0 doi: 10.1016/S0735-1097(97)00324-0 DOI: https://doi.org/10.1016/S0735-1097(97)00324-0
[17]. Laufs U, La Fata V, Plutzky J, Liao JK. Upregulation of endothelial nitric oxide synthase by HMG CoA reductase inhibitors. Circulation. 1998;97(12):1129–35. https://doi.org/10.1161/01.CIR.97.12.1129 DOI: https://doi.org/10.1161/01.CIR.97.12.1129
[18]. Rogler G, Lackner KJ, Schmitz G. Mevalonate is essential for growth of porcine and human vascular smooth muscle cells in vitro. Basic Res Cardiol. 1995;90(6):443–50. https://doi.org/10.1007/BF00788536 DOI: https://doi.org/10.1007/BF00788536
[19]. Nègre-Aminou P, Van Vliet AK, Van Erck M, Van Thiel GCF, Van Leeuwen REW, Cohen LH. Inhibition of proliferation of human smooth muscle cells by various HMG-CoA reductase inhibitors; comparison with other human cell types. Biochim Biophys Acta - Lipids Lipid Metab. 1997;1345(3):259–68. https://doi.org/10.1016/S0005-2760(96)00184-1 DOI: https://doi.org/10.1016/S0005-2760(96)00184-1
[20]. Notarbartolo A, Davì G, Averna M, Barbagallo CM, Ganci A, Giammarresi C, et al. Inhibition of thromboxane biosynthesis and platelet function by simvastatin in type IIa hypercholesterolemia. Arterioscler Thromb Vasc Biol. 1995;15(2):247–51. https://doi.org/10.1161/01.ATV.15.2.247 DOI: https://doi.org/10.1161/01.ATV.15.2.247
[21]. Mayer J, Eller T., Brauer P, Solleder E, Sch~ifer RM, Keller E, et al. Effects of long-term treatment with lovastatin on the clotting system and blood platelets. Ann Hematol. 1992;64:196–201. DOI: https://doi.org/10.1007/BF01696223
[22]. De Oliveira Fernandes Miranda CT, Duarte VHR, Cruz MSDM, Duarte MKRN, De Araújo JNG, Santos AMQS Dos, et al. Association of Serum Alpha-Tocopherol and Retinol with the Extent of Coronary Lesions in Coronary Artery Disease. J Nutr Metab. 2018;2018(Cvd). https://doi.org/10.1155/2018/6104169 DOI: https://doi.org/10.1155/2018/6104169
[23]. Pastor RF, Repetto MG, Lairion F, Lazarowski A, Merelli A, Carabetti ZM, et al. Supplementation with resveratrol, piperine and alpha-tocopherol decreases chronic inflammation in a cluster of older adults with metabolic syndrome. Nutrients. 2020;12(10):1–11. https://doi.org/10.3390/nu12103149 DOI: https://doi.org/10.3390/nu12103149
[24]. Singh U, Jialal I. Anti-inflammatory effects of α-tocopherol. Ann N Y Acad Sci. 2004;1031(Cvd):195–203. https://doi.org/10.1196/annals.1331.019 DOI: https://doi.org/10.1196/annals.1331.019
[25]. Rodriguez-Duarte J, Galliussi G, Dapueto R, Rossello J, Malacrida L, Kamaid A, et al. A novel nitroalkene-α-tocopherol analogue inhibits inflammation and ameliorates atherosclerosis in Apo E knockout mice. Br J Pharmacol. 2019;(2019):757–72. https://doi.org/10.1111/bph.14561 DOI: https://doi.org/10.1111/bph.14561
[26]. Vahedi P, Rajabzadeh A, Soleimani A. An evaluation of the effects of ascorbic acid on the endothelium of coronary and aorta arteries in lead-intoxicated rabbits. SAGE Open Med. 2022;10. https://doi.org/10.1177/20503121221105330 DOI: https://doi.org/10.1177/20503121221105330
[27]. Heriansyah T, Dimiati H, Hadi TF, Umara DA, Kumboyono K. Ascorbic Acid vs Calcitriol in Influencing Monocyte Chemoattractant Protein-1 , Nitric Oxide , Superoxide Dismutase , as Markers of Endothelial Dysfunction : In Vivo Study in Atherosclerosis Rat Model. Vasc Health Risk Manag. 2023;19(March):139–44. DOI: https://doi.org/10.2147/VHRM.S401521
[28]. Pisaniello AD, Psaltis PJ, King PM, Liu G, Gibson RA, Tan JT, et al. Omega-3 fatty acids ameliorate vascular inflammation: A rationale for their atheroprotective effects. Atherosclerosis [Internet]. 2021;324(March):27–37. Available from: https://doi.org/10.1016/j.atherosclerosis.2021.03.003 doi: 10.1016/j.atherosclerosis.2021.03.003 DOI: https://doi.org/10.1016/j.atherosclerosis.2021.03.003
[29]. Alfaddagha, Abdulhamied Elajamib TK, Salehb M, Mohebalib D, Bistriana BR, Welty FK. An omega-3 fatty acid plasma index 4% prevents progression of coronary artery plaque in patients with coronary artery disease on statin treatment. Atherosclerosis. 2019;285(1):153–62. https://doi.org/10.1016/j.atherosclerosis.2019.04.213.An DOI: https://doi.org/10.1016/j.atherosclerosis.2019.04.213
[30]. Omar ZA, Montser BA, Redaarahat MA. Effect of High-Dose Omega 3 on Lipid Profile and Inflammatory Markers in Chronic Hemodialysis Children. Saudi J Kidney Dis Transplant. 2019;30(3). DOI: https://doi.org/10.4103/1319-2442.261337
Downloads
Published
Issue
Section
License
Copyright (c) 2025 Physical Activity, Nutrition and Health Sciences Journal

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
CC Attribution-NonCommercial-ShareAlike 4.0